What is an epiretinal membrane?
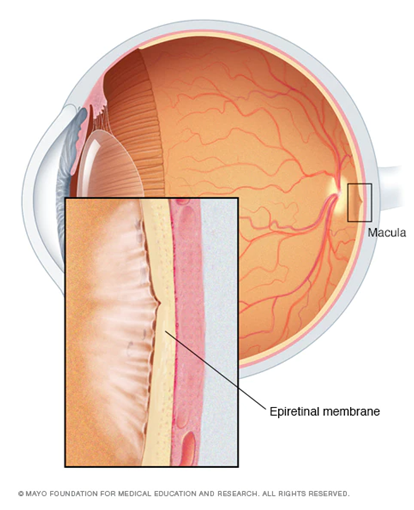
An epiretinal membrane (ERM), also known as cellophane maculopathy or macular pucker, is a thickening of scar tissue that occurs on the inner surface of the retina, a layer of light sensitive tissue that lines the back of the eye. This membrane is made up of glial cells, which are naturally occurring cells in the eye. Due to the formation of the membrane, it can cause the retina to crinkle and disrupt its normal smooth contour.
This overview will cover the global problem of ERM, how it develops, the common symptoms of ERM, the ways that it is diagnosed, and the treatment options for ERM.
The global problem of epiretinal membranes
Epiretinal membranes (ERMs) are a pervasive problem worldwide. An estimated 30 million people in the United States alone are affected by this condition [1]. The prevalence of ERMs in one study suggests that they are higher in certain ethnic populations: Chinese (39.0%), Hispanics (29.3%), white Caucasians (27.5%) and black Africans (26.2%) [1].
How do epiretinal membranes develop?
The exact mechanism by which ERMs develop remain largely unknown despite extensive laboratory studies. Most ERMs do not have a cause and are therefore labelled as being idiopathic. Their occurrence increases with age.
There is some association with ocular diseases such as [1]:
● Posterior vitreous detachment
● Diabetic retinopathy
● Retinal vein occlusion
● Retinal detachment
● Inflammatory eye disease (uveitis)
● Previous intraocular surgery, for example, cataract
There is also some suggestion of systemic associations with [1]:
● Diabetes (even in the absence of diabetic retinopathy
● Smoking
● Hypercholesterolaemia
● Atherosclerosis
What are the symptoms of an epiretinal membrane?
As most ERMs are symptomatic when affecting the macula, the back of the eye responsible for central vision, the symptoms experienced will be noticed when doing activities such as reading or watching television.
Symptoms that may occur include [1]:
● Visual impairment (reduced visual acuity)
● Metamorphopsia (distortion)
● Micropsia (where objects appear smaller in the affected eye)
● Monocular diplopia (shadowing or doubling of images in one eye)
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is an epiretinal membrane diagnosed?
An ERM is diagnosed in a similar way to other eye conditions. An ophthalmologist uses a slit lamp with a special condensing lens which allows visualisation of the retina. On examination, an ERM is discernible for its cellophane-like sheen – also known as the cellophane macular reflex or in more severe cases can show quite thickened preretinal fibrosis [1].

Figure 2. Patient getting eyes checked by eye health professional using a slit lamp.
Multimodal imaging using special equipment such as an optical coherence tomography (OCT) scan – to image the retinal structures — have also been pivotal in obtaining photos of early ERM formation as well as documenting progression over time. This may also be useful in diagnosing associations of ERM, which include cystoid macular oedema or lamellar hole.
What are the treatment options for an epiretinal membrane?
Many epiretinal membranes are amenable to observation and indeed the vast majority of patients are asymptomatic. If the patient is asymptomatic, then there is no need for surgical intervention and the lack of treatment will not generally lead to blindness. Patients may, however, find symptoms of the epiretinal membrane disruptive for everyday life if it is significant enough and therefore opt for surgical management. Currently, there are no other management options besides surgical intervention.
The surgery of choice is a vitrectomy supplemented by an epiretinal membrane peel and can be performed at any hospital with a vitreoretinal service. It is usually performed under local anaesthesia. The vitreoretinal surgeon inserts small ports into the eye which allows access to the vitreous cavity. The vitreous is removed using special intraocular equipment. The epiretinal membrane is dyed for visualization and then gently peeled using very fine forceps. Air is usually left in the eye for several days.
Prognosis after surgery is generally better with shorter duration to symptoms prior to surgery [2]. Recurrence of ERM is thought to be about 1% [3].
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
[1] C. H. Ng et al., “Prevalence and Risk Factors for Epiretinal Membranes in a Multi-Ethnic United States Population,” Ophthalmology, vol. 118, no. 4. pp. 694–699, 2011. doi: 10.1016/j.ophtha.2010.08.009.
[2] A. I. M. Miguel and A. Legris, “Prognostic factors of epiretinal membranes: A systematic review,” J. Fr. Ophtalmol., vol. 40, no. 1, pp. 61–79, Jan. 2017.
[3] O. P. Gupta, G. C. Brown, and M. M. Brown, “A value-based medicine cost-utility analysis of idiopathic epiretinal membrane surgery,” Am. J. Ophthalmol., vol. 145, no. 5, pp. 923–928, May 2008.