What is sub-conjunctival haemorrhage?
A sub-conjunctival haemorrhage is bleeding which occurs under the conjunctiva of the eye. The conjunctiva is the outer skin of the eye, which is a thin layer of clear tissue and is located over the white part of the eye and lines the inside of the eyelids. It is a very common eye condition and occurs when blood vessels under the conjunctiva are broken. Usually, sub-conjunctival haemorrhage is not serious and will resolve on its own. Rarely, it can be a sign of serious trauma.
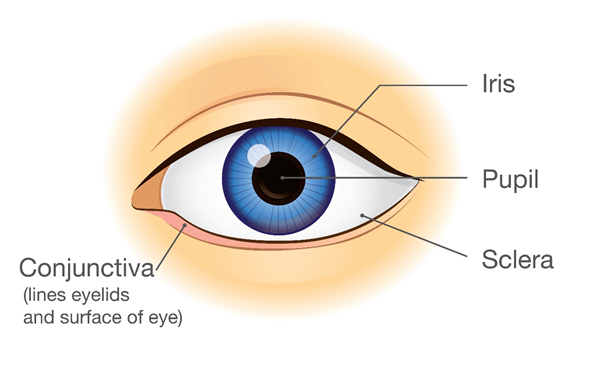
Figure 1. Anatomy of the eye
The following overview will cover the causes of sub-conjunctival haemorrhage, its common signs and symptoms, rogression of sub-conjunctival haemorrhage, diagnosis and treatment options as well as how it can be prevented.
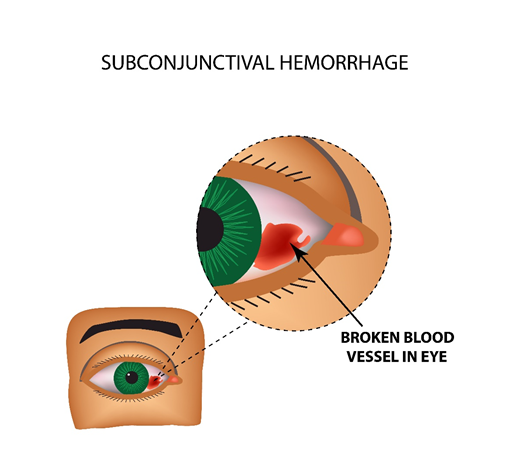
Figure 2. Eye showing sub-conjunctival haemorrhage
Causes of sub-conjunctival haemorrhage
There are several reasons that may cause sub-conjunctival haemorrhage, which include:
• Eye rubbing: Eye rubbing is one of the most common causes of sub-conjunctival haemorrhage and can be triggered by dry or irritated eyes.
• Coughing or straining: Severe coughing or sneezing can cause sub-conjunctival haemorrhage, as can straining while on the toilet or vomiting.
• Trauma causing injury: This can range from mild trauma due to a small foreign body, for example, a particle of grit irritating the eye, to serious trauma from high velocity injuries such as firearm injuries.
• Blood thinning medications: Medications such as aspirin, clopidogrel, warfarin or apixaban can increase the risk of sub-conjunctival haemorrhage, either following mild injury or spontaneously.
• High blood pressure: High blood pressure can increase the risk of sub-conjunctival haemorrhage, either following mild injury or spontaneously.
• Blood clotting disorders: Health conditions in which there is difficulty in clotting blood can increase the risk of sub-conjunctival haemorrhage.
• Recent surgery: It is common for sub-conjunctival haemorrhage to occur following eye surgery, for example cataract surgery.
• Conjunctivitis: Eye infections causing conjunctivitis which is the inflammation of the conjunctiva can rarely also cause sub-conjunctival haemorrhage.
What are the common symptoms and signs of uveitis?
An obvious sign of sub-conjunctival haemorrhage is waking up and noticing that the white of the eye is red. This is usually caused by unintentional eye rubbing while asleep.
Other symptoms include:
● Red eye
● Irritated eye
● Feeling that something is in the eye
● Eye swelling
● Mildly blurred vision
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How can sub-conjunctival haemorrhage progress?
Sub-conjunctival haemorrhage will resolve on its own and does not tend to progress unless there are untreated medical conditions, such as high blood pressure, that can cause increased risk of sub-conjunctival haemorrhage. Those with conditions such as chronic cough or blood-clotting disorders can increase the risk of recurrent sub-conjunctival haemorrhage.
How is sub-conjunctival haemorrhage diagnosed?

Figure 3. Patient getting eyes checked by an eye health professional with a slit lamp
Sub-conjunctival haemorrhage is diagnosed by an eye health professional based on a comprehensive eye check. Questions are asked regarding overall health and any recent injuries to work out the cause of the sub-conjunctival haemorrhage and an eye examination is performed using a slit lamp (a microscope used to look at the eye) to have a closer look at the structures at the front of the eye.
How is sub-conjunctival haemorrhage treated?
Usually, sub-conjunctival haemorrhage will resolve on its own over the course of 1 to 2 weeks. There is no treatment that can speed up its recovery but there is no danger in the eye being red during this time. If it does not resolve on its own after 1 to 2 weeks seek medical advice from an eye health professional or a medical doctor. The eye may be mildly irritated while the sub-conjunctival haemorrhage is present, and your eye health professional may prescribe lubricant eye drops to improve comfort.
Can sub-conjunctival haemorrhage be prevented?
Treating of conditions that increases the risk of sub-conjunctival haemorrhage can help to prevent it, for example, treating dry eyes, managing chronic cough and controlling high blood pressure.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
